Introduction
Chimeric Antigen Receptor (CAR) T cell therapy has improved outcomes for relapsed and/or refractory (r/r) B cell lymphomas. Bridging therapy might be needed in some patients for disease control while CAR T product is being produced. Radiation therapy is known to control the growth of lymphoma and modulate tumor microenvironment, however use of this therapy in the setting of CAR T cell therapy has not been well described. In the present study, we report the efficacy and toxicities of patients treated with a dose of radiation that is lower than previously described for bridging in lymphoma and compare efficacy and toxicities to patients treated with chemotherapy bridging or without bridging therapy.
Methods
We retrospectively compared rates of toxicities and outcomes of 82 patients treated with FDA approved CD19-directed CAR T cells at our institution between November 1, 2018 and April 1, 2020. This study was conducted with approval from the City of Hope National Medical Center Institutional Review Board.
All patients received standard lymphodepleting chemotherapy (LDP) regimen with cyclophosphamide and fludarabine followed by infusion of CAR T cells at day 0. Clinical response was determined 28-35 days following cell administration. Median dose of radiation treatment was 24 Gy (range 4 - 44) in 1.8 - 2.25 Gy fractions. Chemotherapy regimens were at provider discretion.
Results
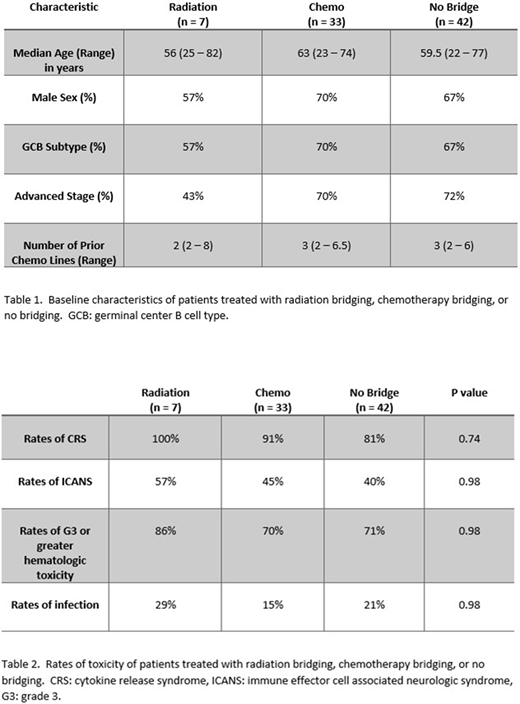
From our institutional database of 82 patients, a total of 7 patients received radiation as bridging therapy. All received the predefined radiation doses with no significant immediate complications. Target organs included the head and neck (4), limbs (2), and chest wall. Structures threatened by the progressing disease included neurovascular (4), limb threatening (2), and major organ threatening (5). All threatened sites were preserved with the use of radiation therapy. 72% of patients receiving RAD had disease that was primary refractory to chemotherapy. The characteristics of patients treated with radiation bridging (RAD) were similar to those treated with chemotherapy bridging (CB) or without bridging (NB), except that patients treated with RAD tended to have less extensive disease (table 1). The adverse rates of CAR T treatment emergent toxicity (CRS, neurotoxicity, hematologic toxicity, or infectious rates) in the RAD group were 83%, 50%, 83%, and 33% respectively. These are comparable to the CB or NB groups (table 2).
Response rates were similar among the three groups with ORR 86% for RAD, 88% for CB, and 93% for the NB group (p = 0.98). Rates of progressive disease were the lowest in the RAD group (14%), followed by NB (21%) and CB (42%) after a median follow up of 241 days (range 43 - 785), however this did not reach statistical significance (p = 0.44).
Discussion
In the present study we demonstrate real world rates of toxicities in patients receiving bridging chemo or bridging radiation. The rates of toxicities were similar regardless of the type of bridging that was utilized. In addition, there was no statistically significant difference in response or relapse rates among the different groups. There was a trend toward lower relapse rates among those treated with radiation. Importantly, this trend was seen even though the majority of radiation doses given were lower than previously described for this indication. Importantly, the vital structures that were threatened by lymphoma were effectively preserved with the utilization of radiation therapy in this setting even with the majority of cases having primary chemo-refractory disease. Additional studies using higher patient number will be needed to strengthen this observation. Our study also sets the stage for future prospective studies optimizing the role of radiation in CAR T cell therapy.
Shouse:Kite Pharma: Honoraria, Speakers Bureau. Budde:Mustang Therapeutics: Research Funding; Merck: Research Funding; Amgen: Research Funding; Kite, a Gilead Company: Consultancy; Gilead Sciences: Consultancy; Roche: Consultancy; AstraZeneca: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal